For 50% of Women Mammograms aren’t Enough
Early breast cancer detection is the strongest chance a woman* has in surviving the diagnosis. The data on stage of diagnosis and mortality is jarring. Early detection at Stage I portends a 99% survival whereas the survival when diagnosed at Stage III or IV plummets to 66% and 27% respectively. On April 30, 2024 the United States Preventive Task Force (USPTF) changed the recommended screening age for mammograms to 40 years old from 45 due to the rising incidence of breast cancer in younger women and to attempt early detection to address the disparities of black women being disproportionately affected both in incidence and mortality. The recommendation is for screening with a mammogram every two years.
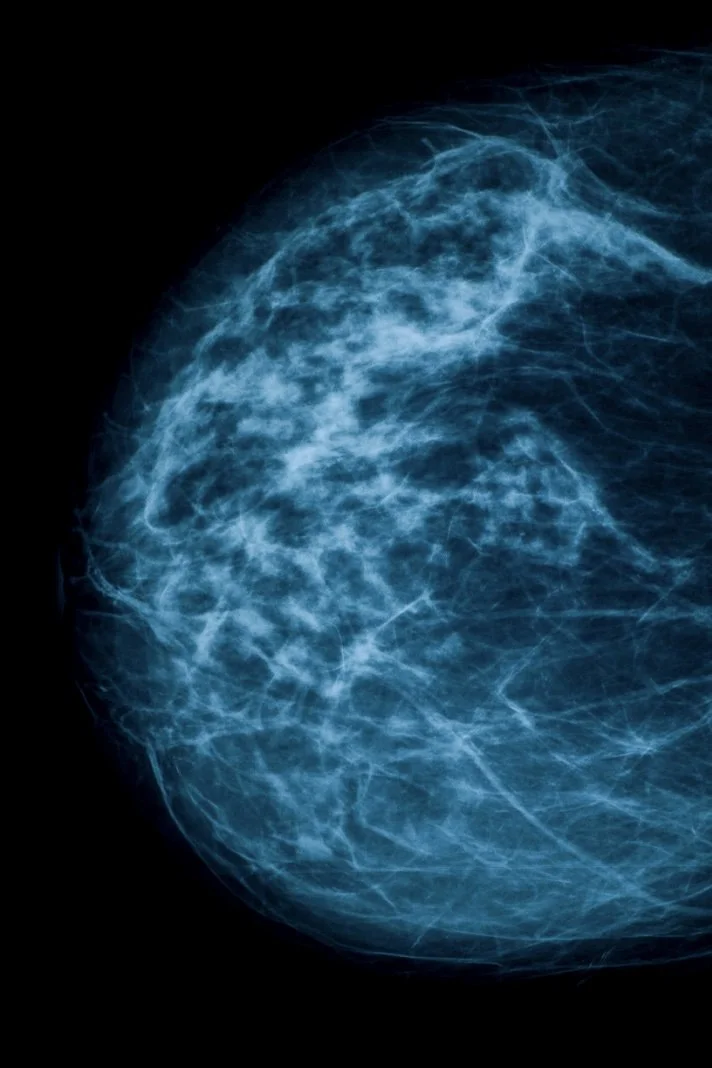
The problem is that for 50% or more women with dense breasts, this is not sufficient for early breast cancer detection and there is no mandate that more sensitive screening tools be covered by insurance to assure early cancers are not missed in these women. Mammograms are great for detecting calcified lesions and modalities such as breast MRI (magnetic resonance imaging) and US (ultrasound) are much better at detecting soft masses (in combination with mammography the sensitivity can be 100%). For women with dense breasts some radiologists liken trying to find cancer on a mammogram as “trying to find a snowball in a snowstorm.” Because glandular tissue that has yet to turn to fat shows up as white on mammograms (the same color as cancer) mammograms will not be evaluable in 40-50% of breast tissue. In 2023, the FDA published a rule stating that mammogram reports sent to patients must include breast density, which would be described as either “not dense” or “dense” which took affect on September 10, 2024. However, once informed of this, there are no further recommendations or mandates to cover screening for these women. Essentially, they receive a letter saying “your mammogram looks negative but you have dense breasts so we’re not sure it's negative. We’ll try again next year.” There is a rising number of women with “normal mammograms” within this context that ultimately are diagnosed with advanced breast cancer.
“There is a rising number of women with “normal mammograms” within this context that ultimately are diagnosed with advanced breast cancer. ”
In reality, these women should subsequently undergo either breast MRI or breast US to increase the sensitivity of early breast cancer detection but there is no requirement to do so. Some radiologists will recommend additional screening and many will not comment beyond the breast density. There is no standard. The USPSTF states that they can’t make additional recommendations on any additional testing without evidence because there are no randomized controlled trials showing MRI will save more lives even though The American College of Radiology supports MRI as the preferred test for women with dense breasts and breast radiologist strongly express that it will save lives. Without randomized controlled trials, the USPSTF will not make recommendations and without USPSTF recommendations, insurance companies won’t approve coverage. For the majority of women who are not informed by the health care system of what screening they should actually undergo and who are unable to pay out of pocket for it, medicine, and to a greater extent the insurance companies, are failing women at risk for missed early detection of breast cancer and imposing a higher mortality if diagnosed at a later stage. Even with new technology and studies in the works, it will still take years to materialize in to USPSTF recommendations leaving women vulnerable to late stage diagnosis of breast cancer that we have every possibility of preventing. Dr. Daniel Kopans, professor emeritus of breast radiology at Harvard’s Massachusetts General Hospital stated that “ If we did MRI as the routine screening for everyone, we probably would save [almost] everyone from breast cancer.”
There are arguments that the system cannot support both practically and financially providing every woman with dense breasts an MRI . There are also down sides to providing a highly sensitive screening test to all women, some of whom may not need them: when you have high sensitivity in a test, you are at risk for false positives possibly leading to unintended additional imaging or biopsies. Through precision medicine, we can identify the women who would benefit from additional screening and prioritize early detection rather then passively allowing late stage breast cancer diagnoses to persist leading to preventable lives lost.
“Through precision medicine, we can identify the women who would benefit from additional screening and prioritize early detection rather then passively allowing late stage breast cancer diagnoses to persist leading to preventable lives lost. ”
One potential tool for some women with higher risk of breast cancer is the risk-score called the Tyrer-Cuzick risk score. If you have ≥ 20% lifetime risk of breast cancer according the calculator, annual screening with mammography offset every 6 months with annual breast MRI is recommended and should be covered by insurance. I am grateful for my primary care physician who astutely knew to do this. As a women with extremely dense breasts and a negative mammogram, I asked a member of my care team to order a breast MRI. She was happy to but stated it wouldn’t be covered and that because most of my family members with breast and other cancers were in their 60’s when diagnosed it didn’t pose a higher risk to me. When I met my new primary care physician, she said that wasn’t necessarily the case and we walked through the Tyrer-Cuzick risk score which placed me at a 29% lifetime risk of breast cancer. One month later, I underwent my first screening MRI, had met with a genetic counselor and a high risk breast clinic provider who would be in charge of navigating my lifetime process of breast cancer screening. As a healthy active woman, I felt both humbled by the risk and grateful for the opportunity for early and appropriate screening with a dedicated team. I also immediately recognized the privilege I have as a well informed longevity physician who advocated for myself and the access to multiple dedicated care teams I am afforded. Even with all this and insurance coverage, the out-of-pocket cost is still substantial and out of reach for the majority of women in this country.
Identifying women at higher risk for breast cancer through precision medicine with equitable and sensitive screening access should be the standard of care. Some types of cancer are difficulty to diagnose early. Breast cancer is not one of those. No woman should be diagnosed with breast cancer beyond Stage I. We have the science and we have the tools now, why wait?
If you are interested in learning more about your cancer risk, advanced technology for cancer screening and prevention through the lens of longevity medicine, I would love to discuss this more with you.
In the meantime, live vividly.
Java Tunson, MD
*For the purposes of this article please note when using the word woman, it refers to those assigned female at birth.